Categories more
- Adventures (16)
- Arts / Collectables (15)
- Automotive (37)
- Aviation (11)
- Bath, Body, & Health (76)
- Children (6)
- Cigars / Spirits (32)
- Cuisine (16)
- Design/Architecture (21)
- Electronics (12)
- Entertainment (4)
- Event Planning (5)
- Fashion (44)
- Finance (9)
- Gifts / Misc (6)
- Home Decor (44)
- Jewelry (40)
- Pets (3)
- Philanthropy (1)
- Real Estate (14)
- Services (22)
- Sports / Golf (14)
- Vacation / Travel (60)
- Watches / Pens (14)
- Wines / Vines (24)
- Yachting / Boating (16)
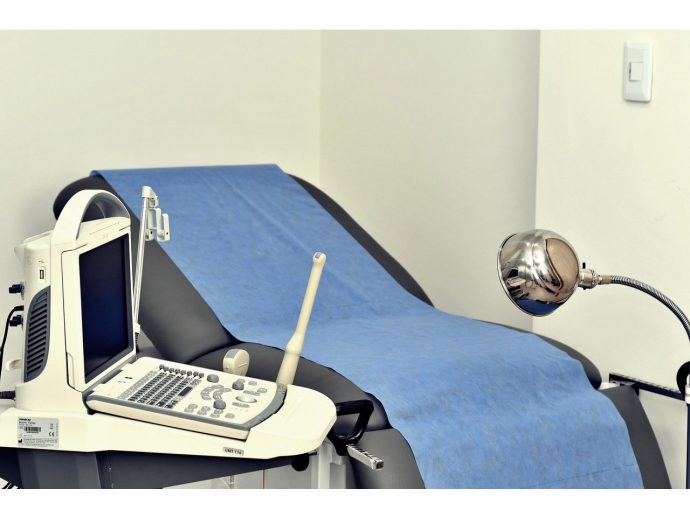
Why Communities Rely on OB-GYN NPs During Health Resource Shortages
Published
08/21/2025In many parts of the country, health resource shortages have shifted the weight of patient care onto providers who can adapt quickly and deliver specialized services without delay. Among these providers, OB-GYN nurse practitioners (NPs) have emerged as indispensable figures. Their ability to offer comprehensive reproductive and women’s health care in both urban and rural settings allows communities to maintain access when hospitals or clinics face staffing gaps.
The demand for these professionals has surged as health systems contend with physician shortages, budget limitations, and patient volumes that strain capacity. OB-GYN NPs bring advanced clinical training, the capacity to prescribe, and a patient-centered approach that often bridges the gap between limited resources and urgent needs. Their scope of practice in many states enables them to work freely or in collaboration with physicians, making them a flexible solution for strained health networks.
Communities rely on these practitioners not only because of necessity but because of trust. In regions where patients may otherwise travel long distances or endure weeks of waiting for specialized care, OB-GYN NPs provide consistency, immediacy, and a level of personalized attention that patients value deeply. Their role extends beyond clinical care into patient advocacy, health education, and community engagement.
Bridging Access Gaps in Underserved Areas
One of the most visible contributions OB-GYN NPs make is ensuring that underserved populations maintain consistent access to reproductive and gynecological services. In rural towns where hospitals have shuttered maternity wards, these practitioners often operate as the only specialized resource for prenatal visits, contraception counseling, and preventive screenings. Without them, patients would face geographic and financial barriers that significantly limit care.
Their work aligns with broader efforts to close disparities in women’s health. Targeted community health initiatives focus on improving access and equity in reproductive care to strengthen reproductive outcomes and counteract the impact of care deserts. Evidence from these initiatives shows that expanding NP roles in reproductive health improves outcomes and reduces delays in treatment, particularly for communities far from major hospitals.
Furthermore, OB-GYN NPs often partner with community organizations to conduct mobile clinics, outreach events, and education sessions. These initiatives are particularly critical in areas where transportation and insurance coverage are major obstacles. By bringing services directly to patients, they not only close care gaps but also establish a model of proactive, preventive health delivery.
Mitigating Physician Shortages in High-Demand Specialties
Physician shortages in obstetrics and gynecology have created a care bottleneck that OB-GYN NPs are uniquely positioned to ease. Their training equips them to manage a broad range of cases from routine exams to certain complex conditions, allowing physicians to focus on patients with more specialized or acute needs. This redistribution of workload improves patient flow and reduces wait times across the system.
In hospital and clinic settings, OB-GYN NPs frequently handle prenatal check-ins, postnatal care, and follow-up visits, freeing physicians for surgeries, high-risk deliveries, or other specialized interventions. In doing so, they act as both an independent provider and a collaborative partner, ensuring that care remains continuous despite fluctuating staffing levels.
This collaboration is especially valuable during crisis periods such as flu seasons, pandemic surges, or local emergencies when staffing shortages can be severe. The capacity of NPs to step into expanded roles during these times prevents service interruptions and sustains quality standards that communities depend on.
A Focus on Preventive Care and Early Intervention
While much attention is given to acute and emergency care, preventive services are equally critical in maintaining public health. OB-GYN NPs are instrumental in ensuring that women receive regular screenings for cancers, sexually transmitted infections, and other conditions that can be addressed more effectively if caught early.
Their patient-centered approach allows them to spend more time discussing lifestyle, family planning, and risk factors with patients. This education fosters an environment where women feel empowered to take control of their reproductive health and make informed decisions. By focusing on prevention, OB-GYN NPs help reduce the long-term costs and burdens on the healthcare system.
In many communities, preventive care from NPs is the difference between a treatable condition and a life-threatening diagnosis discovered too late. Their consistent presence and emphasis on early detection translate into better health outcomes and a more resilient healthcare infrastructure.
Expanding Scope Through Telehealth and Mobile Services
The integration of telehealth into OB-GYN NP practice has expanded their reach into communities that previously had limited or no access to specialized care. Video consultations, remote monitoring, and digital prescription services enable them to manage follow-ups, provide counseling, and monitor patients without requiring travel.
Mobile health units operated or staffed by OB-GYN NPs further break down barriers by physically bringing care to neighborhoods and towns lacking facilities. These mobile services are often coordinated with local health departments and non-profit organizations to target the most underserved areas.
The dual strategy of telehealth and mobile care has proven especially effective during resource shortages, when in-person capacity is limited. By leveraging technology and mobility, OB-GYN NPs ensure that no patient is left behind due to distance or logistics.
Building Trust and Cultural Competence
Trust plays a pivotal role in healthcare, particularly in reproductive and women’s health where sensitive topics are involved. OB-GYN NPs are known for cultivating strong provider-patient relationships, often through active listening, empathy, and cultural sensitivity. This rapport is a powerful factor in encouraging patients to seek timely care.
Cultural competence is more than language skills; it involves understanding the social, economic, and cultural factors that shape health behaviors. OB-GYN NPs often undergo training to address these dimensions, enabling them to provide care that aligns with patients’ values and needs.
In diverse communities, this ability to bridge cultural divides leads to higher engagement, better adherence to treatment plans, and improved outcomes. For communities facing shortages, the trust built by these practitioners becomes an irreplaceable asset in sustaining public health.
Preparing for Future Challenges in Women’s Health
Looking ahead, demographic shifts, aging populations, and evolving healthcare policies will continue to shape the demand for OB-GYN NPs. Workforce planning will need to account for their expanding role, particularly in addressing rural and underserved urban areas where shortages are most acute.
Investments in NP education, training programs, and residency-style fellowships can ensure that the next generation of practitioners is ready to meet growing needs. Encouraging legislative changes that support full practice authority in more states will also enhance their ability to serve effectively.
Communities that embrace these measures will be better positioned to maintain robust reproductive health services regardless of economic or logistical constraints. The reliance on OB-GYN NPs during shortages today serves as a blueprint for building a resilient healthcare system for tomorrow.